Predictive analytics is transforming mental health care by using data to predict and prevent crises. It helps identify risks like hospital readmissions, relapse, or suicide attempts with up to 80% accuracy. This approach also improves treatment outcomes, reduces costs, and addresses the growing global mental health crisis.
Key Insights:
- Global Crisis: Nearly 1 billion people live with mental disorders, costing economies billions annually. Access to care remains a challenge, with up to 90% untreated in some regions.
- Predictive Power: Models forecast outcomes like suicide attempts with AUC scores of 0.82–0.89 and reduce hospital readmissions by 15–20%.
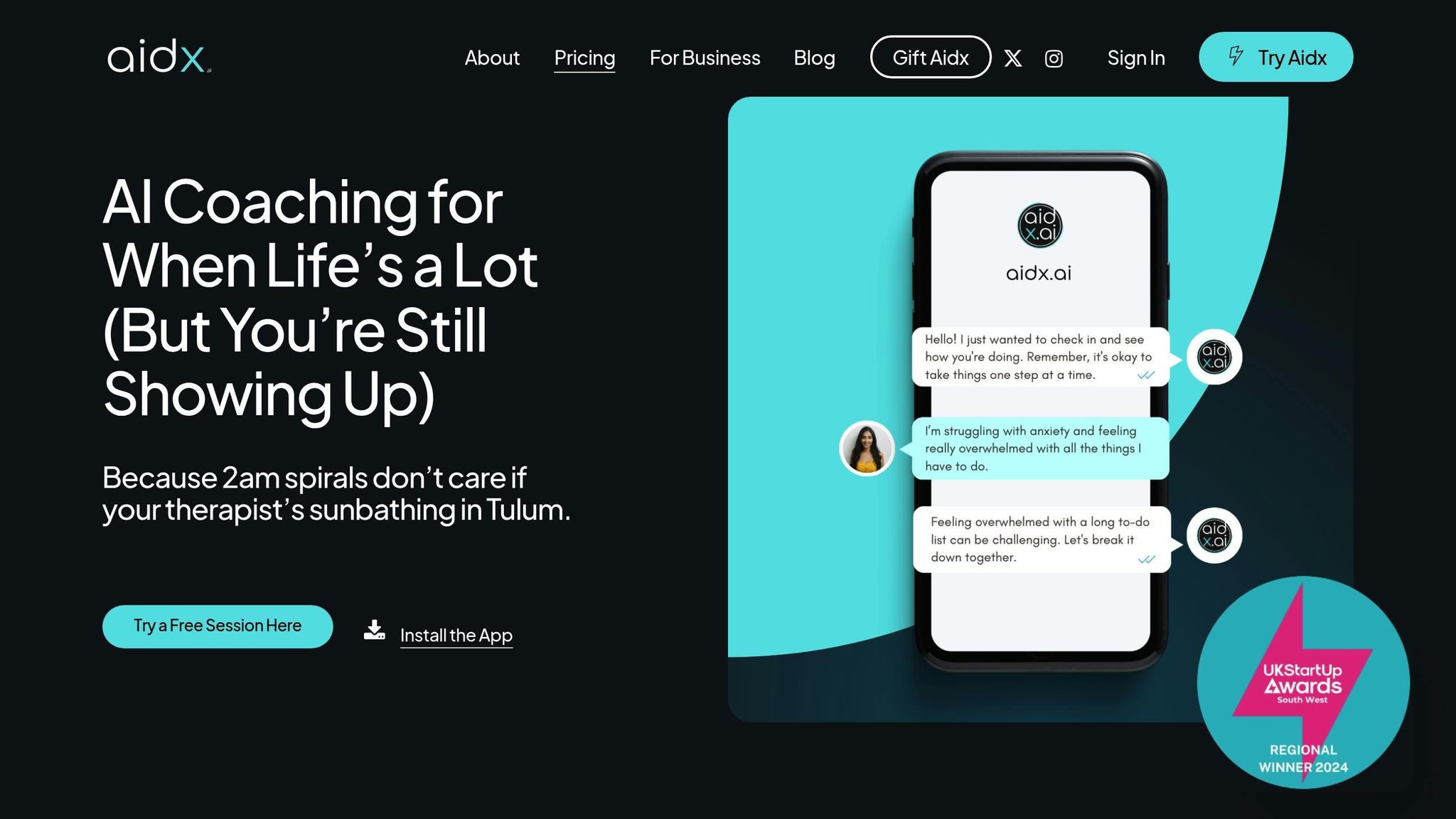
- Technology Requirements: Cloud computing, data security, and AI-driven platforms (like Aidx.ai) enable scalable solutions, offering personalized care via apps, chatbots, and real-time data analysis.
- Ethics and Privacy: Ensuring equity, reducing bias, and protecting sensitive data are critical to scaling predictive analytics responsibly.
By combining AI, real-time data, and scalable frameworks, predictive analytics is reshaping mental health care globally, offering proactive and personalized support to underserved populations.
The relationship between big data and predictive analytics in mental health
Infrastructure and Technology Requirements for Scaling
Expanding predictive analytics on a global scale demands a solid technological foundation capable of managing large volumes of data securely and efficiently. This goes beyond just computing power – it includes cloud platforms, secure data storage, seamless integration across systems, and real-time data processing. Let’s break down the key technological elements that make this possible.
Core Infrastructure Requirements
At the heart of scalable predictive analytics lies cloud computing, which provides the computational muscle and storage capacity needed for global operations. As Rema Padman, Trustees Professor at Carnegie Mellon University‘s Heinz College, puts it:
"I think cloud computing is really the base requirement in place because of the computational power and data storage that are needed to make this work at scale" [6].
Healthcare organizations are increasingly moving to cloud-native platforms, which not only improve data integration but also reduce costs [6].
Data security is another critical piece of the puzzle, especially when dealing with sensitive mental health information. Recent statistics reveal that 78% of healthcare organizations experienced cybersecurity incidents last year, with financial losses ranging from $100,000 to $1,000,000 [4]. More than 60% reported disruptions to care delivery as a result [4].
Interoperability is also a major hurdle. Currently, only 55% of hospitals can electronically access patient information from external sources, and just 40% can integrate that data into their electronic health records (EHRs) without manual intervention [5]. This lack of integration undermines the effectiveness of predictive analytics.
To address this, Health Information Exchanges (HIEs) are evolving. These platforms are becoming cloud-native, API-enabled, and AI-enhanced, allowing for real-time data aggregation, smoother integration with mobile tools, and secure collaboration among healthcare providers [5].
AI-Driven Platforms for Scalable Mental Health Support
AI-powered platforms are transforming the delivery of mental health support worldwide. These systems must combine advanced analytics with user-friendly interfaces while adhering to strict privacy and security standards.
A key factor in global scalability is multi-platform accessibility. For example, Aidx.ai provides evidence-based mental health support through multiple channels, including web apps, WhatsApp, and Telegram. By offering users the ability to choose their preferred communication method, barriers related to technology adoption and digital literacy are significantly reduced.
Cloud-based AI platforms offer immense scalability. One Medical, for instance, has used Amazon Web Services (AWS) since 2007 to provide virtual care, secure messaging, and on-demand video consultations. Deepak Alur, Vice President of Engineering at One Medical, highlights the benefits:
"AWS enables One Medical to automate tasks in the cloud by providing scalable infrastructure for machine learning workflows…Automation reduces manual work, enhances efficiency and supports seamless operations" [6].
Security and compliance are integral to these platforms. IBM Watson Health integrates AI solutions with a HIPAA-compliant cloud infrastructure, ensuring data security while streamlining regulatory compliance [10]. Similarly, JPMorgan Chase‘s AI-powered assistant, used by 60,000 employees, demonstrates how large-scale AI deployments can improve efficiency, reduce errors, and enhance compliance [10].
The growing reliance on AI for cybersecurity is reflected in market trends, with the global AI cybersecurity market projected to reach $13.80 billion by 2028. A 2023 Gartner survey also found that 60% of compliance officers plan to invest in AI-driven regulatory technology by 2025 [9].
Data Integration and Real-Time Analytics
Effective predictive analytics rely on seamless data integration and real-time processing. These capabilities enable proactive mental health interventions and personalized care adjustments, helping to prevent crises before they escalate.
Measurement-Based Care (MBC) exemplifies this approach. The NHS Talking Therapies Program, launched in 2008, has collected self-reported data from 98% of its users, creating a rich dataset for improving care quality. This initiative has boosted clinical recovery rates from 38% to 52%, with every £1 invested yielding £4 in reduced healthcare costs and increased productivity [3].
Advanced analytics systems can process multiple data streams simultaneously. For example, HealthArc combines digital behavioral health assessments with analytics to identify issues, assign risk scores, and send real-time alerts [7]. These systems integrate data from various sources, including patient-reported outcomes, demographic details, and natural language processing.
Organizations are also adopting unified analytics platforms for better data management. Community Health Network’s migration to Azure Databricks in 2024 is a prime example. Dr. Patrick McGill, the network’s Chief Transformation Officer, explains:
"Dynamics really helps us work toward that goal of deeply knowing our patients, their preferences, when they’re interacting with the system, when they’re coming into the system, any gaps in care they might have or challenges they might experience" [6].
To manage diverse data types – ranging from wearable devices to social media interactions – data pipeline architecture must be robust. Sameer Sethi from Hackensack Meridian Health notes:
"Having data in the cloud makes development of data and analytics assets and connectivity a lot easier and faster" [6].
Automation is also playing a growing role. By 2024, AI-powered tools are expected to automate 70% of tasks related to classifying Personally Identifiable Information (PII), a critical step for ensuring privacy while enabling comprehensive data analysis [9].
Finally, privacy-preserving technologies are crucial. Techniques like data anonymization, enhanced auditing, and proactive risk management ensure compliance with regulations such as HIPAA. Striking the right balance between innovation and privacy protection requires sophisticated solutions that safeguard sensitive mental health data without compromising functionality.
Data Sources and Model Development in Predictive Analytics
Accurate mental health predictions depend on a mix of diverse data sources and well-designed predictive models. The quality and variety of the data directly influence the reliability of these models, while proper validation ensures they work effectively across different populations and environments.
Key Data Sources for Mental Health Analytics
High-quality data forms the backbone of mental health predictive analytics, drawing from a range of sources to create more accurate predictions than any single data type could provide.
- Surveys and interviews: These remain central to mental health analytics, capturing self-reported symptoms, demographic details, and clinical assessments. For instance, the Connecticut Behavioral Health Partnership (CBHP) created a shared database in 2006, integrating over 100 variables, including demographics and healthcare utilization. Using 18 specific variables, their predictive models achieved an 80% accuracy rate in identifying individuals likely to stay engaged in treatment [1].
- Digital communication data: Social media posts and text messages provide valuable insights into mental health states. Natural language processing (NLP) analyzes these communications to detect emotional patterns and psychological indicators.
- Audio data: Voice recordings can reveal stress, depression, or anxiety through analysis of tone, context, frequency, and timing.
- Sensor and wearable device data: Devices like smartwatches, smartphones, EEG monitors, and MRI scanners track behavioral and physiological patterns, such as sleep habits and physical activity, offering continuous monitoring.
- Multimodal data integration: Combining information from video, sensors, and other sources allows for a more comprehensive understanding of mental health conditions, improving predictive accuracy [8].
| Data Type | Examples | Collection Methods |
|---|---|---|
| Surveys and interviews | Questionnaire responses, interviews | Quantitative and qualitative data collection |
| Social media and text | Social media posts, text messages | NLP to analyze emotional and psychological patterns |
| Audio data | Speech samples, recordings | Analysis of voice tone, context, and timing |
| Sensor and device data | Smartwatch data, EEG, MRI | Continuous tracking of physiological responses |
| Multimodal data | Video, multiple sensor inputs | Integration of diverse data streams |
Developing and Validating Predictive Models
Once diverse, high-quality data is available, the focus shifts to building and validating predictive algorithms. The success of these models depends on choosing the right algorithms, thorough training, and rigorous testing across various groups. Machine learning techniques have shown promise in mental health applications, provided they’re developed and validated carefully.
A 2021 review reported that predictive analytics models achieved 70–80% accuracy in predicting psychiatric hospital readmissions, suicide risks, and treatment responses [2]. In a U.S. Department of Veterans Affairs-funded study, machine learning algorithms predicted suicide attempts with AUC scores between 0.82 and 0.89 [2].
- Random Forest algorithms: These have been particularly effective in mental health predictions. For example, they achieved:
- 80% accuracy in predicting depression among international students in the UK.
- 95.1% accuracy in forecasting bipolar disorder hospital admissions in Colombia.
- 88.8% accuracy among Rwandan youth [11].
These results highlight the algorithm’s ability to perform well across different demographics and regions.
Incorporating demographic and cultural factors into model design enhances their precision. Tailoring questionnaires and analytical methods to reflect these variations leads to better outcomes. Additionally, transfer learning – where pre-trained models are adapted for specialized tasks – has shown high success rates even with smaller datasets [8].
Predictive models also have a tangible clinical impact. When integrated with electronic health record systems, they can reduce hospital readmissions by 15–20%, improving patient outcomes and cutting costs [2].
Data Privacy and Compliance
After building reliable models, ensuring data security becomes a top priority. Handling sensitive mental health data demands strict privacy measures and adherence to regulations like HIPAA in the U.S. and GDPR in the EU. For example, GDPR allows data deletion upon request, whereas HIPAA requires retaining health information for six years [12].
The financial risks of data breaches are steep. Since 2020, healthcare data breach costs have risen by 53.3%, reaching an average of $10.93 million in 2023 [13]. To mitigate these risks, organizations must implement strong technical safeguards:
- Encryption: Techniques like AES-256 protect data at rest and in transit.
- De-identification: Methods such as data masking, pseudonymization, and the OMOP Common Data Model protect patient identities while preserving data utility [14].
- Access controls: Role-Based Access Control (RBAC) and Multi-Factor Authentication (MFA) restrict access to authorized personnel only.
- Regular audits: Security checks and vulnerability assessments help identify and address weaknesses.
Federated learning is emerging as a privacy-preserving solution. It trains machine learning models on decentralized data, ensuring raw data remains on local devices while improving overall model performance [13][14].
Data minimization is another critical practice. Organizations should only collect and retain the data necessary for their analysis. Clear policies for data usage, storage, and retention, supported by comprehensive governance frameworks, are essential.
Platforms like Aidx.ai demonstrate how privacy-first approaches can support mental health initiatives globally. By offering evidence-based therapy through secure channels like WhatsApp and Telegram, Aidx.ai ensures accessibility while maintaining strict privacy protections.
sbb-itb-d5e73b4
Policy, Ethics, and Equity in Scaling Predictive Analytics
Scaling predictive analytics in mental health goes beyond just building strong infrastructure and integrating data. It requires navigating a maze of regulations, ethical considerations, and equity concerns. Organizations must strike a balance between advancing technology and safeguarding vulnerable populations while adhering to varying legal frameworks worldwide.
Understanding the Regulatory Landscape
Regulations governing mental health predictive analytics differ widely across the globe. For example, the Law Library of Congress highlights that about 40 jurisdictions have specific legislation addressing AI, each with its own rules and standards [16].
In the United States, mental health data privacy is primarily governed by HIPAA. Meanwhile, the European Union takes a broader approach with GDPR and the newer EU AI Act. The AI Act classifies systems by risk level, requiring high-risk applications, such as those used in mental health, to undergo fundamental rights impact assessments. These regulations not only impose compliance requirements but also provide clearer guidance for ethical development [16].
Regional differences also play a role. For instance, AI-based medical devices are often approved in Europe before gaining clearance in the U.S., which can influence global rollout strategies. As technology evolves, regulatory frameworks must adapt to keep pace [16]. These complexities set the stage for addressing ethical challenges in deploying predictive analytics.
Managing Ethical Challenges
Ethical concerns are a significant hurdle in scaling mental health predictive analytics. AI systems trained on biased datasets can unintentionally reinforce disparities in diagnosis and treatment, especially for marginalized communities [36–38]. To address this, organizations should:
- Diversify training datasets.
- Conduct regular bias audits.
- Form multidisciplinary teams that include clinicians, data scientists, ethicists, and community representatives [15].
Transparency is also critical. Many AI systems function as "black boxes", making it hard to understand how recommendations are generated. Clear communication about how these systems work can build trust among patients and clinicians [35–37].
| Ethical Challenge | Impact | Mitigation Strategy |
|---|---|---|
| Algorithmic Bias | Disparities in diagnosis and treatment | Use diverse datasets, fairness techniques, and ongoing monitoring |
| Lack of Transparency | Erodes trust | Offer clear explanations and publish transparency reports |
| Data Privacy Concerns | Risk of misuse of sensitive information | Implement robust encryption, anonymization, and strict access controls |
Informed consent becomes more complex with AI-driven systems. Patients need to know how their data will be used and understand the technology’s capabilities and limitations [35–38]. Transparency reports that detail model development, validation, and performance in plain language can further enhance trust. Additionally, maintaining clinical oversight ensures that AI supports rather than replaces professional judgment.
Promoting Equity and Inclusion
Equity in mental health predictive analytics requires addressing systemic barriers and embracing diverse perspectives. The goal is not just to avoid harm but to actively promote fair and inclusive outcomes.
Engaging a wide range of stakeholders – physicians, patients, and community members – early in the development process is crucial [17]. As Llana James, a post-doctoral fellow at Queen’s University, points out:
"Race-medicine is not solely about Black people, it is also about how White people have used themselves as a primary reference in clinical assessment, and have in so doing, not necessarily tended to the precision of the science." [17]
Bias monitoring, or algorithmovigilance, should be an ongoing effort to prevent discriminatory outcomes throughout the AI lifecycle [17]. Addressing social determinants of health – like housing, education, and employment – also helps ensure that these technologies do not perpetuate existing inequities.
Training datasets must reflect a broad spectrum of ethnic, racial, gender, age, and socioeconomic backgrounds to account for diverse experiences and cultural contexts [17]. Digital health tools also offer opportunities to improve equity. For instance, digital connectivity can break down physical barriers, making mental health services more accessible in remote or underserved areas. However, this only works if solutions address disparities in digital literacy, device access, and internet connectivity [18].
Platforms like Aidx.ai demonstrate how inclusive design can expand access. By offering evidence-based mental health support through familiar channels like WhatsApp and Telegram, Aidx.ai lowers barriers such as the need for specialized apps. Its 24/7 availability and multilingual support further enhance accessibility for diverse populations.
To maintain equity as systems scale, continuous evaluation is essential. Organizations should measure whether their solutions effectively serve target populations and adapt as needed. Bias mitigation must remain a priority throughout the product lifecycle to ensure long-term positive outcomes [17].
Implementation Strategies and Future Trends
Scaling predictive analytics for mental health requires strong frameworks, seamless integration with AI, and a forward-looking approach to emerging trends. By adopting proven strategies and staying informed about industry advancements, organizations can expand access to effective mental health support worldwide.
Frameworks for Scaling Predictive Analytics
The backbone of any predictive analytics system is its infrastructure. Predictive models rely on high-quality, diverse data to deliver accurate insights. This means organizations need to combine information from various domains and stakeholders to create comprehensive health profiles.
Take the Connecticut Behavioral Health Partnership (CBHP) as an example. In 2006, CBHP united multiple state agencies to oversee behavioral healthcare for over 800,000 Medicaid beneficiaries. They developed a shared database containing more than 100 variables, including demographics, service usage, and healthcare costs across medical, behavioral, dental, and pharmacy services. This comprehensive approach allowed CBHP to predict treatment engagement with 80% accuracy [1].
Healthcare facilities that have implemented machine learning-based predictive systems have seen notable improvements. For instance, patient readmission rates dropped from 18.2% to 12.7% over two years, and predictive models enhanced clinical decision-making by 27.3% compared to traditional methods [22].
Key to success is assembling multidisciplinary teams that include data scientists, engineers, and clinicians [21]. Organizations also need to invest in secure, scalable data infrastructure with efficient pipelines for managing and analyzing data. Regular monitoring and updates ensure these systems remain accurate and effective over time.
Another compelling example is Carelon‘s suicide prevention program, launched in 2018. By utilizing predictive models, the program reduced suicidal events by over 20% and cut behavioral health costs by 30% [1]. These frameworks, combined with AI technologies, amplify the impact of mental health support systems.
Integration with AI-Powered Platforms like Aidx.ai
AI platforms are transforming mental health care by offering real-time monitoring and personalized interventions, extending support beyond traditional clinical settings.
Platforms like Aidx.ai showcase how advanced therapeutic intelligence can scale evidence-based interventions. Aidx.ai’s Adaptive Therapeutic Intelligence (ATI) System™ uses techniques from CBT, DBT, ACT, and NLP to tailor responses based on users’ emotional states, goals, and interaction history. This allows for highly personalized support through voice-enabled conversations, notifications across multiple channels, and integrated planning tools.
The combination of predictive analytics and AI platforms unlocks critical capabilities. For example, AI-driven monitoring can detect early signs of mental health deterioration, enabling timely interventions [19]. By analyzing large datasets, AI provides actionable insights and can predict suicide attempts with an accuracy of 92% for the next week and 85% for the next two years [24]. When paired with platforms like Aidx.ai, which offer immediate support, these predictive tools create life-saving early intervention systems.
AI-powered platforms not only improve care but also address global workforce shortages, making them an essential component of modern mental health infrastructure.
Emerging Trends in Predictive Analytics
Looking ahead, several emerging trends are poised to reshape the landscape of mental health predictive analytics, offering exciting opportunities for growth and innovation.
- Federated Learning: This method enables healthcare organizations to build advanced predictive models without sharing sensitive patient data. It ensures compliance with privacy regulations while leveraging insights from global datasets [20].
- Natural Language Processing (NLP): Advances in NLP are making it easier to extract valuable insights from unstructured data such as clinical notes, patient feedback, and conversation transcripts, improving the accuracy of predictions [20].
- AI and IoT Integration: Wearable devices are increasingly being used to provide real-time data for health predictions. These devices can monitor mood, stress levels, sleep patterns, and more, supporting precise and timely interventions [47, 55].
- Personalized Medicine: By combining genomic data, electronic health records, and lifestyle information, predictive analytics is enabling highly tailored treatment recommendations at scale [20]. This shift aligns with the rapid growth of digital mental health solutions, with the mental health app market projected to reach $17.5 billion by 2030 [24].
- Telehealth Expansion: Between 2019 and 2021, telehealth usage surged from 15.4% to 86.5%, opening new avenues for predictive analytics to enhance remote mental health care [23].
"To achieve a high-performing company, you need resilient, healthy employees." – Tim Munden, Unilever’s chief learning officer [24]
As these trends continue to evolve, predictive analytics will play a pivotal role in creating integrated, personalized, and scalable mental health solutions that can meet the needs of diverse populations while maintaining high-quality care.
Conclusion
Predictive analytics is reshaping how we approach mental health care, offering data-driven tools for early intervention. When paired with real-time EHR notifications, these technologies can forecast outcomes with an impressive 70–80% accuracy. They also reduce readmissions by 15–20% and improve recovery rates by 25% – a game-changer for both patient outcomes and healthcare costs. Considering that inpatient psychiatric hospitalizations in the U.S. average over $5,000 per stay, the financial advantages of proactive care are hard to ignore [2].
"Behavioral health systems powered by big data analytics can function more efficiently and deliver vast enhancements to the overall quality of care available to any population… The enhancements fuelled by big data analytics enable us to build health systems that invest strategically and can better reduce mental health crises and disparities across the US."
- Jeremy Weisz, CEO and Co-Founder of Greenspace Health [3]
The NHS Talking Therapies Program is a prime example of how technology and human oversight can work hand in hand. Since 2008, its session-by-session outcome monitoring has boosted clinical recovery rates from 38% to 52%, while delivering an estimated $4 in returns for every $1 invested. These returns stem from lower healthcare costs and higher productivity [3].
Platforms like Aidx.ai are at the forefront of this shift, combining evidence-based therapeutic methods with predictive analytics to move mental health care from reactive to proactive. This approach allows for identifying individuals at risk days or even weeks before a crisis and delivering timely, personalized interventions [2].
As we look ahead, the future of mental health care depends on three key areas: building strong infrastructures capable of handling diverse data and real-time analytics, establishing ethical frameworks that safeguard privacy and equity, and developing scalable solutions to reach underserved populations. This is especially critical given that 75% of the global mental and behavioral disorder burden falls on low and lower-middle-income countries [25]. By focusing on these areas, we can create a system that not only addresses immediate needs but also builds a foundation for long-term mental health equity.
FAQs
How can predictive analytics improve mental health care and lower costs on a global scale?
Predictive analytics is changing the game in mental health care by identifying individuals at risk of crises before they escalate. By examining data such as electronic health records, these models can anticipate potential mental health challenges, giving healthcare providers the chance to intervene early. This proactive approach doesn’t just help patients avoid severe episodes and hospitalizations – it also eases the financial burden on healthcare systems by reducing the reliance on emergency and inpatient care.
Beyond crisis prevention, predictive analytics is streamlining mental health services by improving resource allocation and treatment planning. This ensures that care is not only more efficient but also more effective, paving the way for mental health support that is easier to access and more affordable for people everywhere.
What ethical and privacy considerations are important when scaling predictive analytics for mental health?
When expanding the use of predictive analytics in mental health, addressing ethical concerns and ensuring privacy protections are non-negotiable. Ethical considerations should cover areas like obtaining informed consent, safeguarding confidentiality, and minimizing bias in how data is collected and used. On the privacy side, the focus must be on protecting sensitive health information, preventing unauthorized access, and avoiding any misuse of data.
To achieve this, organizations need to adopt strong data protection measures and make patient privacy a top priority. Steps like anonymizing data, keeping security protocols up to date, and staying alert to new technological risks are critical. Transparency and accountability also play a big role, with clear regulatory guidelines needed to ensure mental health data is handled responsibly and ethically.
How can AI-powered platforms make mental health support more accessible and personalized, especially in underserved areas?
AI-driven platforms are transforming mental health support by making it more accessible and tailored to individual needs. Using tools like predictive analytics, natural language processing, and virtual therapy, these technologies offer round-the-clock assistance through chat-based services and teletherapy. This is especially valuable for people in remote or underserved regions where connecting with mental health professionals can be challenging.
By analyzing user data, AI can design personalized interventions that improve engagement and deliver better outcomes. Many of these platforms also break down language and cultural barriers by providing multilingual support, making services more inclusive for diverse communities. This approach not only fills critical gaps in care but also ensures that mental health support reaches those who might otherwise go without it.



